Dealing with a breast cancer diagnosis is devastating. Your oncologist will help you determine the best way to fight the cancer through surgery, radiation or chemotherapy. But once those decisions are made, what can you do to feel “whole” again? While reconstruction is not mandatory, many women find that opting for a “new” breast or breasts helps restore their body image and put the disease behind them.
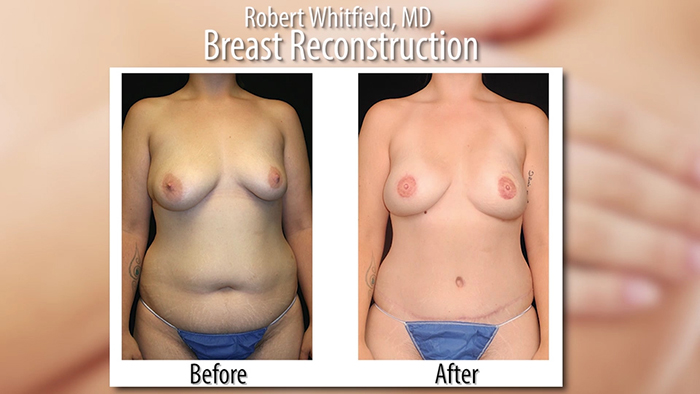
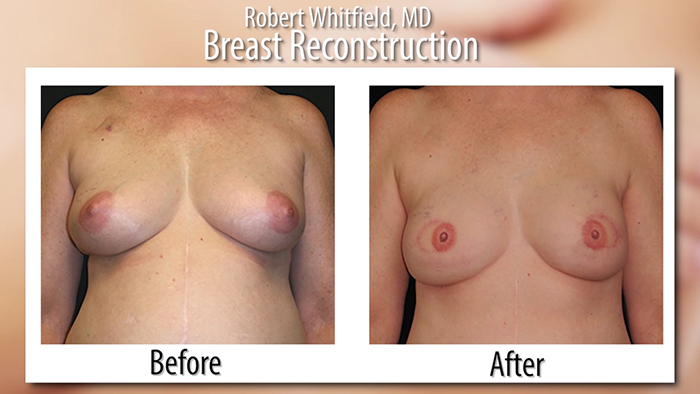
New medical techniques and devices make it possible for surgeons to create a breast that mimics a natural breast in both form and appearance. Dr. Robert Whitfield at the Breast and Body Center in Austin, Texas is a specialist in the latest procedures. “We are a little unique in that although we do aesthetic surgery, a large component of our practice is taking care of women with breast cancer.” Dr. Whitfield’s philosophy is that a reconstructed breast should be no less aesthetic than a breast enhancement. “It’s one of the most rewarding surgeries we perform.”
by Isabel Bolt
and Robert Whitfield, MD
A Question of Timing
Frequently, reconstruction is possible immediately following breast removal (mastectomy), so the patient wakes up with a breast mound already in place, having been spared the experience of seeing herself with no breast at all. Most mastectomy patients are medically appropriate for reconstruction, many at the same time that the breast is removed. The best candidates, however, are women whose cancer, as far as can be determined, seems to have been eliminated by mastectomy. More news to keep in mind—in 1998 the Federal Breast Reconstruction Law was passed which requires all health insurance companies cover reconstruction of the breast on which mastectomy has been performed and surgery and reconstruction of the other breast to produce a symmetrical appearance. Breast reconstruction can be performed at the same time as the mastectomy OR be delayed until you heal from your mastectomy and complete additional cancer treatments.
Tissue Expanders — Implant Surgery
The use of a breast implant for reconstruction almost always requires a tissue expander. According to Dr. Whitfield, this has historically been the most common technique. “A tissue expander and empty saline implant is placed in the breast at the time of the mastectomy. Over time the implant is filled with saline through an internal valve until the chest area is stretched sufficiently to place a permanent silicone implant in place of the saline one. It’s a 2-stage technique.” The filling usually takes 4-6 months. Dr. Whitfield advises his patients to wait approximately 3 months after the final fill before placing the permanent implant. “You want all the tissues to heal around the device in case you want to refine or alter the breast at the final reconstruction surgery.”
Dr. Whitfield is particularly excited about a new type of expander called Artoura™. “We used to have quite limited options with the available expander sizes. Because of its design, Artoura™ is perfect for petite women.” Artoura is the first and only expander capable of providing precisely controlled pocket formation for more predictable expansion outcomes designed to prevent unwanted dimensional changes for more consistent results.
Flap Surgery — Using your Own Tissue
Autologous reconstruction uses tissue from another place on your body to form a breast shape. The tissue, called a “flap”, usually comes from the belly, the back, buttocks, or inner thighs to create the reconstructed breast. According to Dr. Whitfield, advancements in microsurgery have made it easier to perform nerve and muscle sparing procedures—but requires very experienced microsurgeons who routinely do these cases.
Whitfield and his partner Dr. Ned Snyder at the Breast and Body Center of Austin are proud to be one of the pioneers in these techniques and have done over 1000 cases over the last decade. Free flaps require your plastic surgeon to have skill in microsurgery, which involves attaching the blood vessels from the tissue flap to the vessels in the chest area so that the new breast gets sufficient blood supply.
Not all surgeons are trained in this type of surgery. Dr. Whitfield calls it, “the most natural form of reconstruction. If someone wants to use their own tissue for breast reconstruction, I use the exact same incision as I would for a tummy tuck. I take that tissue and leave it connected to blood vessels of the abdomen that run right through rectus muscle. The tissue is carefully removed fully intact and transferred to the chest and hooked up to the vessels we use for heart surgery. Once those are attached, the tissue is like your own transplant—we’ve just moved it from the tummy to the chest.” After the transfer, Dr. Whitfield shapes the new breast. Abdominal tissue is similar to breast tissue, so it makes a good substitute and can feel quite natural.
Thin women may not have the choice of using their own tissue, nor do women having a bilateral procedure because there simply is not enough skin. In either implant or autologous reconstruction, further surgical techniques can use grafting/tattooing to simulate the nipple and areola.
One Stage – Skin and Nipple Sparing
Immediate reconstruction has the obvious advantage of enabling you to wake up from the surgery “complete.” In some select cases nipple sparing mastectomy can be performed which preserves the nipple, areola and the breast skin. Essentially, only the tissue inside your breast is removed—the shell of your natural breast are left intact. A silicone implant is placed where your tissue used to be. The result can resemble a breast augmentation. Dr. Whitfield agrees that nipple sparing surgery delivers highly aesthetic results, but not everyone is a candidate. “There are a select number of patients for the one stage permanent silicone gel procedure. It is limited to women with early stage breast cancer (stage I or II) and those with a B or C cup with no ptosis. Larger breasted women or those with considerable sag are not good candidates.”
Getting Back to Normal
The creation of a new breast can dramatically improve your self-image, self-confidence and quality of life. Dr. Whitfield emphasizes it is all about patient selection. Remember that the choice is yours, but may be limited to your anatomy and condition. A consultation with a breast reconstruction specialist will properly educate you on the range of options available to you. Be certain you are meeting with a board certified plastic surgeon who is familiar with a variety of techniques. Ultimately, whether you have implant, autologous tissue, or skin and nipple sparing surgery, you will no doubt be grateful to reclaim your body with a restored breast of normal shape, appearance and size. The “fear of the mirror” will vanish along with the dark clouds of your initial diagnosis.














Facebook
Twitter
Instagram
YouTube
RSS