In this special 3 part series of PSC Deep Dive host William P. Adams Jr. MD moderates a group discussion on Breast Implant Associated-Anaplastic Large Cell Lymphoma (BIA-ALCL) with 3 BIA-ALCL patients. Not all physicians and patients are aware of BIA-ALCL, which can lead to delays in diagnosis and progression of the disease. Raising awareness of BIA-ALCL, its symptoms and treatment protocol, is critical to maximizing the safety of patients with breast implants.
What is BIA-ALCL?
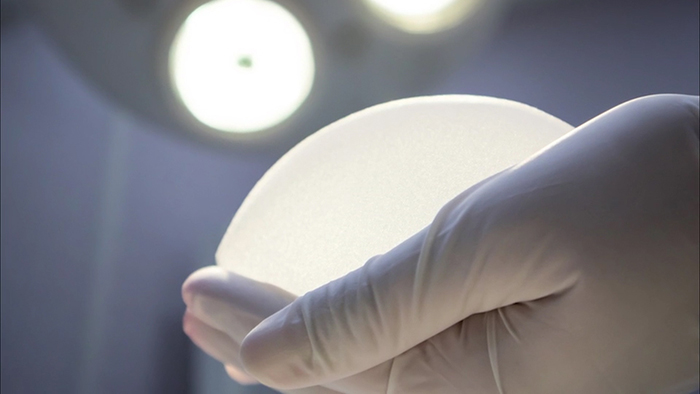
BIA-ALCL is a lymphoma associated with textured breast implants, both saline and silicone. Unlike breast cancer, which develops in the tissues of the breast, BIA-ALCL is found in the fluid and scar tissue surrounding the breast implant. When the disease is detected early, surgical removal of the implant, the scar tissue and the fluid can cure the disease. When the disease is not detected early, it can spread and in some cases, become deadly.
Raising Physician Awareness of BIA-ALCL
Plastic surgeons around the world are collaborating to learn all they can about BIA-ALCL. The topic is front and center at plastic surgery society meetings, educational conferences and in plastic surgery medical journals. While physician awareness in the world of plastic surgery is certainly on the rise, it is not yet where it needs to be. Other physicians – primary care doctors, emergency room doctors and OB/GYN doctors, are often the first line of care for women with breast implants. Many of these physicians are still unaware of the symptoms, methods of diagnosis and treatment for BIA-ALCL.
Raising Patient Awareness of BIA-ALCL
Two years ago a small group of ten women diagnosed with BIA-ALCL joined together in an online support group to share their experiences. Since then, the group has grown to include over two thousand women around the world who have breast implants, approximately one hundred of whom have been diagnosed with BIA-ALCL. What began as a patient support group has now become a platform for raising patient awareness. Thanks to their efforts, women are catching the symptoms earlier and getting proper treatment, and as a result, lives are being saved.
Combining the Efforts of Plastic Surgeons & Patients
The Plastic Surgery Channel invited Terri McGregor, Michelle Forney and Jennifer Cook, all BIA-ALCL patients and moderators of the BIA-ALCL Facebook group to share their stories on the Plastic Surgery Channel with the goal of raising both patient and surgeon awareness.
Michelle’s Story
Michelle was symptomatic for about three years before she learned about BIA-ALCL.
“I had off and on swelling in my right breast, major itching,” describes Michelle. “My itching would wake me up in the middle of the night and I would scratch like crazy. Inside the breast I had pain and aching.”
She first took this list of symptoms to her general practitioner, who referred her to a dermatologist. The diagnosis they gave her was shingles. When the symptoms didn’t subside after a year of treatment, she then went to a plastic surgeon. First, her surgeon thought she was experiencing a very low grade capsular contracture. The symptoms continued and grew worse until she experienced an onset of swelling that occurred approximately ten months ago.
“My right breast got to be the size of a basketball. It was humongous,” she describes. “From there, they finally identified a seroma in Ultrasound.” The fluid was tested for CD-30, and the test came back negative, possibly due to errors in the methods of testing. After a complete bi-lateral capsulectomy, the tests came back positive for BIA-ALCL.
It is only through the empowering of patients, physicians and surgeons with information on the treatment and diagnosis of BIA-ALCL that women like the 3 special guests in this Deep Dive are able to overcome the disease and live healthy lives post-treatment.
Michelle’s History
Symptoms: Pain and aching in Right Breast, Intense itching, on and off swelling; until right breast swelled to the size of a “volleyball”
Time lag to diagnosis: 3 years exactly
Evaluating Clinician: For the 3 years of trying to find out what was wrong, I was evaluated by: OBGYN, Primary Care Physician, Plastic Surgeon and Breast Specialist.
Date of diagnosis: January 28, 2018
Tissue Biopsy: pathologic analysis of tissue capsule after bi-lateral capsulectomy. Following a needle aspiration of fluid prior was not tested correctly which was tested incorrectly by pathology.
Staging: 2A BIA-ALCL
Treatment: Surgical resection
Oncology follow up: Oncology follow up included PET/CT Scan every 4 months while NED for 2 years
Jennifer’s History
Larger breast shape and nominal fluid around implant dismissed as “normal.”
MRI, Mammogram and US performed and no concern for malignancy was identified.
Time lag to diagnosis: 1 year of self-advocacy for concerns
Evaluating Clinician: Radiology initiated testing
Date of diagnosis: August, 2017
Tissue Biopsy: Core Needle Biopsy of Capsule Mass with Implants in-situ
Staging: 2A BIA-ALCL
4 masses identified with PET/CT scan, no LNI, no distant spread. 2 masses behind implant were not identified on US or MRI
Treatment: 2 cycles Brentuximab prior to surgery, Oncology & PS for Explant, 5 cycles of chemotherapy after explant
Oncology follow up: Oncology follow up includes PET/CT every 4 months while NED for 2 years
Terri’s History
Implant: Allergan Natrelle Textured Cohesive Gel 6 years in-situ
Symptoms: No noticeable symptoms prior to routine Mammogram, thought to have caused Implant rupture. Confirmed rupture with MRI
Time lag to diagnosis: N/A, incidental finding during routine rupture replacement due to visible tumors on capsule tissue
Evaluating Clinician: Plastic Surgeon
Date of diagnosis: July, 2015
Tissue Biopsy: Capsule of ruptured implant
Staging: BIA-ALCL Stage 4 due to LNI of axilla and abdomen
Treatment: 6 rounds of CHOEP, 2 rounds of GDP, 4 rounds of Brentuximab, Stem Cell Transplant and 15 rounds of Radiation
Oncology follow up: Every 3 months for 2 years while NED, progressing to 6 month follow ups.
Symptoms of BIA-ALCL
Patients with breast implants need to be aware of the symptoms associated with BIA-ALCL, and visit a board certified plastic surgeon who is knowledgeable on the topic of BIA-ALCL when these symptoms present.
The most common symptom, enlargement of the breasts, is what physicians refer to as a seroma, which is a collection of fluid. A seroma may occur in one or both of the breasts. Sometimes a patient will detect it when a breast becomes enlarged or swollen. Other times the seroma may be detected during ultrasound or medical imaging, such as an MRI taken of the breasts.
“If you have a seroma, that’s not normal,” shares Dr. Adams. “Even if somebody that you see says, ‘Oh, that’s okay.’ It’s really not okay, until it’s evaluated.”
Another symptom associated with BIA-ALCL is the hardening or lumps of the breast or armpit region. Lymph nodes in the armpit or in the breasts may become tender or painful to the touch.
Other less common symptoms women have reported include breast firmness, fever, chills, night sweats, nauseousness and fatigue.
Patient Symptoms:
- Enlargement of one or both breasts
- Breast Firmness
- Lumps in or around the breast/underarm
- New pain or other noticeable changes
- Fever, chills, or night sweats
Diagnosis of BIA-ALCL
When a patient presents with symptoms, further testing needs to be done. Diagnosis of BIA-ALCL is based on a test of the fluid present around the breast implant. The fluid is typcially analyzed for cytology and CD30. Some seromas may be CD30 postive with negative cytology indicating a pre-BIA-ALCL condition. The fluid analysis can make the diagnosis of BIA-ALCL.
Even in cases where the fluid does not test positive for CD30, it is recommended that women with fluid around their breast implants undergo additional testing and remain under the care of their plastic surgeon to manage the care and treatment of their seroma.
Treatment of BIA-ALCL
In 2017 the National Comprehensive Cancer Network (NCCN) established guidelines for the diagnosis and treatment of BIA-ALCL. These guidelines recommend a multi-disciplinary approach. Oncologists and surgeons must work together to care for patients.
Whenever possible, the entire capsule surrounding the implant and fluid must be removed in a procedure referred to as a capsulectomy. The diseased tissue should be removed with clear margins and this is important for complete surgical treatment.
When the disease is caught early and treated with a complete capsulectomy, currently 100% of patients have been cured. In most cases patients are monitored with imaging every three to six months for two years following treatment.
Stay tuned for part 2 and 3 of the series coming soon.